WTF is a PBM???

Today’s letter is the reason I started Drugstore Cowboy in the first place. If you…
Live in the United States
Think our healthcare system sucks
Don’t know what a PBM is
Then you better buckle up. This is the most important thing you will read today.

Meet the Mafia
If you’ve ever filled a prescription in America, you’ve crossed paths with a PBM. You just didn’t know it.
Caremark. Express Scripts. OptumRx.
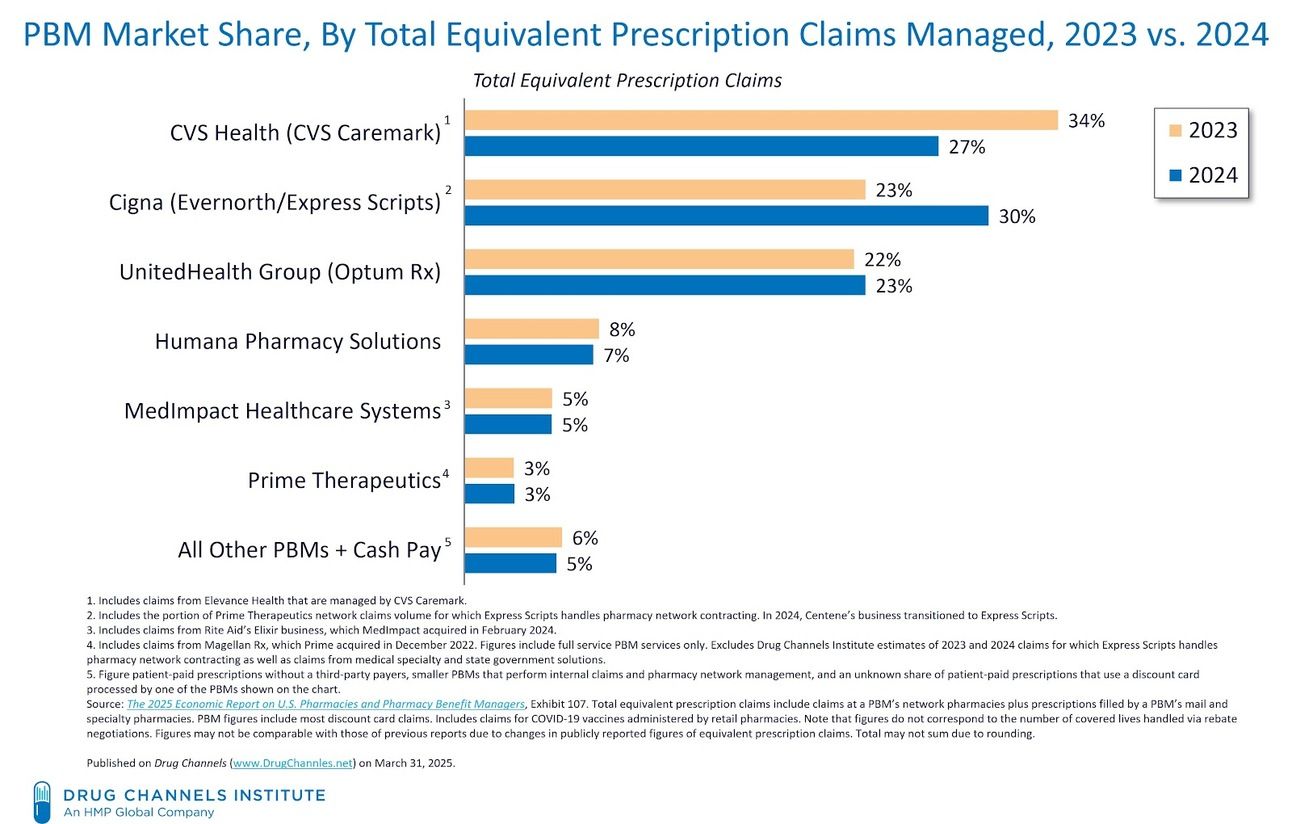
These are the three biggest Pharmacy Benefit Managers (aka PBMs) and they control nearly 80% of the prescription drug market in the United States.
They aren’t drug manufacturers. They aren’t pharmacies. And despite what they say, they definitely aren’t working in your best interest.
In fact, most people have never even heard of them.
But they’re the most powerful players in American healthcare - and the reason your medication costs what it does.
I call them the Mafia because they skim money off every transaction and dare you to question why.
It’s hard to explain how massive these companies are, but I’ll give it a shot. In 2023, it was estimated that the “Big 3” PBMs brought in $456.3 Billion in revenue.
For comparison, in 2023 Microsoft reported $232 Billion, Alphabet (Google) reported $324 Billion, and Apple reported $383 Billion.
And those companies operate globally. These PBMs are not messing around.

So, What Do They Do?
Pharmacy Benefit Managers were originally created to process prescription drug claims for insurance plans.
Today, that barely scratches the surface. They also:
Decide which drugs your insurance covers (your formulary)
Set the copay you pay at the register
Determine how much your pharmacy gets reimbursed
Negotiate secret "rebates" from drugmakers
Pocket a piece (or all) of those rebates
They don’t make the drugs. They don’t fill them. But they control access, pricing, and payment.
That’s not just middleman territory. That makes them the Corleones.


OK… Explain it to Me Like I’m a Fifth-Grader
The most important thing to understand about how PBMs control the industry is their rebate scheme. Here’s how I explain it to my patients at C.O. Bigelow:
OptumRx is hired by a bunch of insurance companies to create the formularies (the list of medications covered by a specific insurance plan) for all of their drug plans.
Let’s say enough insurance companies hire OptumRx that they control 30% of all prescriptions in America. (This is actually true.)
Now, OptumRx goes to the three biggest statin (cholesterol drug) manufacturers:
- AstraZeneca (makes Crestor)
- Pfizer (makes Lipitor)
- Merck (makes Zocor)
And they say:
“We control access to 30% of the statin market. We only need to pick one statin to cover for all of those patients. What are you going to pay us to make sure it’s your drug?”
That’s the billion dollar question. We call that a rebate.
If a drug company doesn’t give the best answer to that question, it loses potential sales to a third of the market. So each company inflates the price of their drug to make room for a juicy rebate that they can hand directly to the PBM.
The PBM pockets part (or all) of it, and makes sure that statin is the one you’re allowed to get when you go to the pharmacy.
None of this has anything to do with what’s best for the patient. It’s about who pays the most to play.
Now multiply this game across every therapeutic category: diabetes, cancer, ADHD, HIV, asthma, etc... Every drug becomes a bidding war. The more desperate the condition, the higher the stakes.
The PBM rebate system is the number one most corrupt game in America. And we all suffer for it.

Who Pays the Price?
Patients
Pay more at the pharmacy
Can’t get the drug their doctor actually wanted to prescribe
Sometimes pay more using insurance than they would with cash
Pharmacies
Are reimbursed less than what the drug costs us
Are forced out of business or squeezed into silence
Employers
Think they’re getting cost savings
Actually fund a rigged system that prioritizes rebate size, not clinical value
Drugmakers
Must play the rebate game or get locked out of the formulary
Can’t drop prices, because then there’s no room for rebates
The Government
Wastes billions of our tax dollars paying insane prices for medications through Medicare and Medicaid
Everyone loses… except Tony Soprano.
Nephron Research estimates PBMs now capture 42 cents of every dollar spent on brand-name drugs in the commercial market. Think about that for a second. A company that provides zero value to you is getting 42% of the cost of your medication.
And what does that lead to? The estimated average prescription cost in the US jumped from $69 in 2014 to $95 in 2024, while the number of scripts filled hasn’t risen at even close to the same rate. That’s the tangible effect of drug companies fighting each other to provide PBMs the largest rebate possible.
We are all stuck in a perverse race to the top to see how much these useless middlemen can suck out of our pockets before the whole system comes crashing down.

Why Didn’t I Know This Before?
Because PBMs like it that way. And everyone with the power to do something about it is getting a piece of the pie to keep quiet.
They hide behind other names:
CVS (owns Caremark)
Cigna (owns Express Scripts)
UnitedHealth (owns OptumRx)
They bury the real costs behind opaque secret contracts.
And they’re vertically integrated:
Caremark controls both the PBM and the pharmacy (CVS)
OptumRx is part of UnitedHealth, the largest insurer in the U.S.
Express Scripts is owned by Cigna
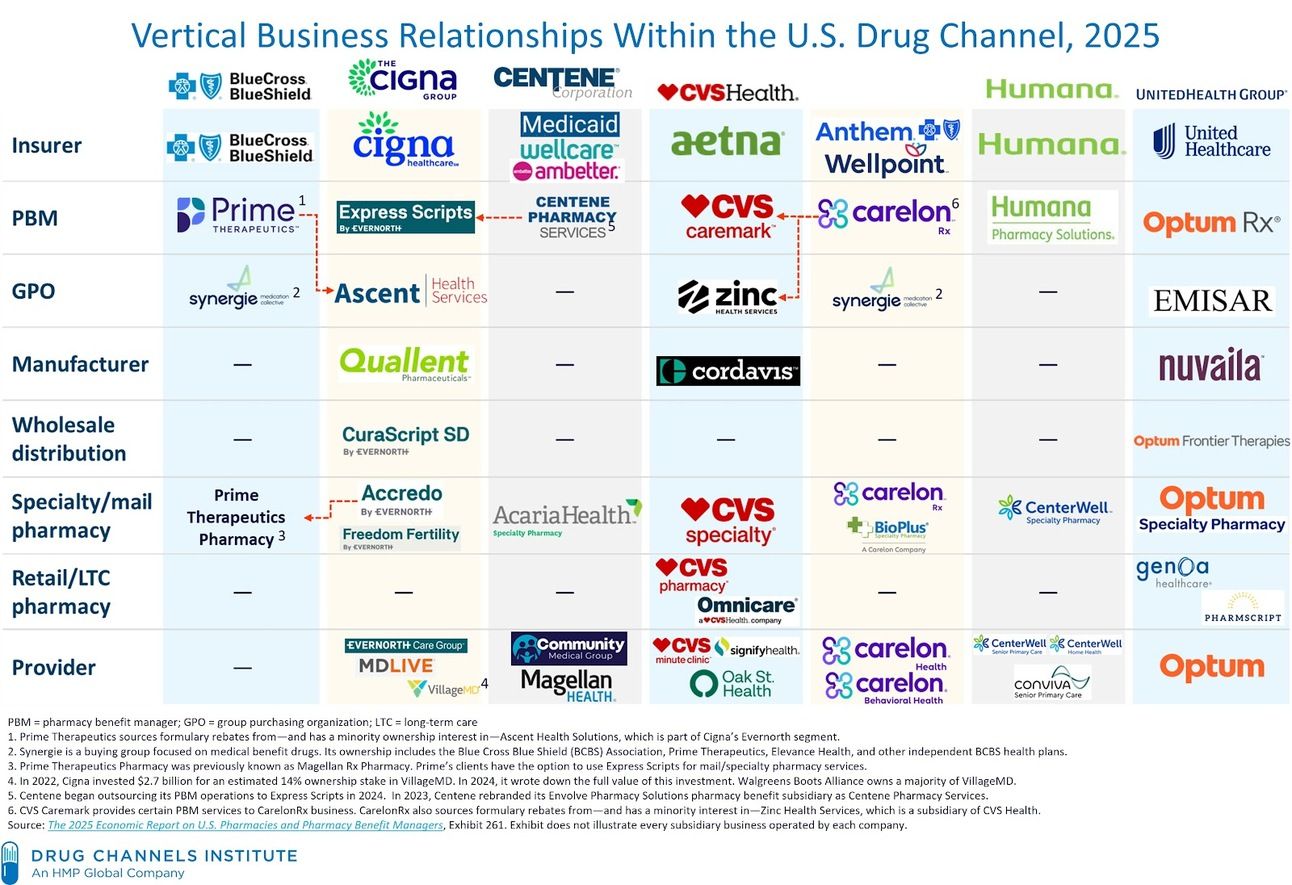
Recognize a pharmacy on this chart that you’ve been forced to use? I bet your PBM owns it!
They are the house, the dealer, and the pit boss. And they’re still telling you the game is fair.
When you walk into the casino at least you already know the odds are stacked against you.
This kind of scheme wouldn’t fly in any other industry. But in healthcare (arguably the most important system in our daily lives) we let it happen. It affects our health, our taxes, and the sustainability of care in this country. And yet, most people still don’t know enough about how it works to fight for real change.
Even lawmakers who want to fix the system can’t easily untangle it. PBMs flood Washington with lobbyists. They spend tens of millions convincing politicians that they’re lowering drug costs, while quietly collecting their cut behind the scenes.
This is how monopolies thrive. Through complexity, confusion, and fear of change.

Final Dose
I’m a fourth-generation pharmacist. I run the oldest pharmacy in America. And I’m telling you: this is the fight that matters. This is why I started this newsletter.
PBMs are draining money from every part of the healthcare system.
They kill independent pharmacies. They warp access to care. They extract money from the sick and call it innovation.
They are robbing us blind right before our eyes. And if we want American healthcare to improve then we need to start shouting about it.
Drugstore Cowboy exists to expose the people behind the curtain. This is only the beginning. What I’ve written today barely scratches the surface on what these companies are doing.
If you just learned all this for the first time, you should be angry. And if I do my job, you’re going to get a lot angrier in the weeks ahead.
So, how can you help change the system?
Listen. Learn. And spread the gospel.
Start by forwarding this to someone you know who needs to hear this. And if someone sent this to you, head to my homepage and subscribe so you can find out more about what we’re up against.
We can’t change what we don’t understand. Let’s start by spreading the truth. This affects all of us. There has to be a better way.
Giddy up.

Alec Wade Ginsberg, PharmD, RPh
4th-Gen Pharmacist | Owner & COO, C.O. Bigelow
Founder, Drugstore Cowboy
